(American College of Lifestyle Medicine)
During my two decades of service in military medicine, I saw the extraordinary demands on U.S. service members. Our military personnel must perform at the maximum level, sometimes under grueling conditions, to accomplish their missions. Their performance, however, does not depend only on superior training or weaponry. It relies on resilience and strong physical and mental health.
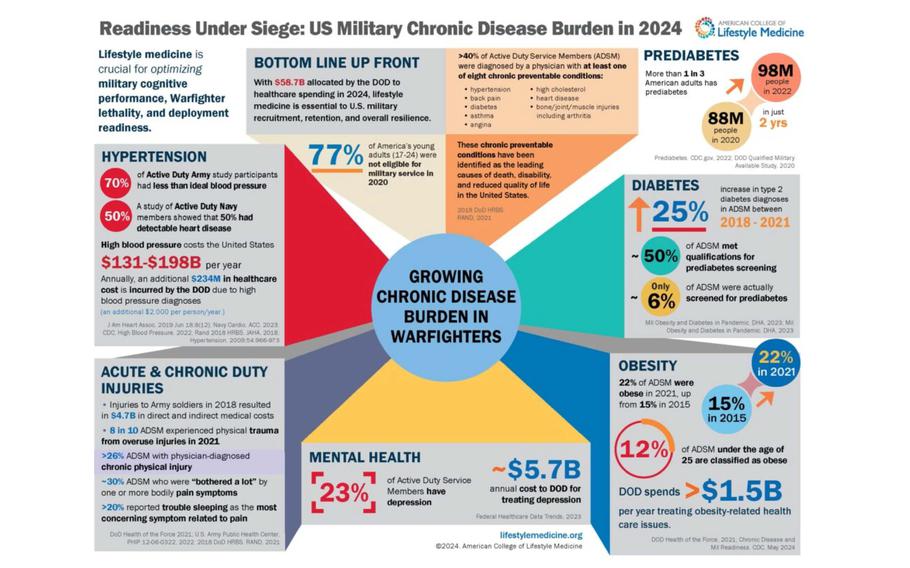
The same lifestyle-related health issues that afflict the rest of the country, such as being overweight, obesity, type 2 diabetes and high blood pressure, are now recognized as immediate threats to the military’s warfighting capabilities and our national security.
First, the growing chronic disease epidemic has created a shrinking pool of eligible recruits — a Pentagon study determined that 77% of young Americans would not qualify for military service without a waiver for being overweight, having other health problems or past drug use.
Second, those who do qualify are more likely to arrive with pre-existing health conditions. In recent years, the Air Force has adjusted training schedules to be less physically intense initially to support conditioning of new recruits and decrease risk of injury.
After basic training, Air Force service members tend to decline in overall health. Prevalence of prediabetes, diabetes and obesity among active members of all the services is growing. One analysis found that low physical activity and physical fitness among Army recruits from the southern states correlated with increased risk of musculoskeletal injuries, which are considered one of the biggest medical impediments to military readiness.
In short, service members with chronic health conditions are more prone to injury and illness, making them less fit to perform their duties. That’s not to mention the significant financial burden — $58.7 billion was allocated for health care spending in 2024 — that managing these primarily preventable conditions places on the military health care system.
To address these growing health challenges, we must embrace new strategies, such as accentuating lifestyle behavior change, to create a culture of health that enables our service members to reach top performance. The military recognizes this. That’s why its newest branch, the U.S. Space Force, recently announced a lifestyle medicine education, training and certification initiative available to all members of the Space Force Guardian Resilience Team, which educates and trains its service members on physical and mental health. Lifestyle medicine, which uses therapeutic lifestyle interventions as a primary modality to treat chronic conditions, applies six pillars: optimal nutrition, physical activity, restorative sleep, stress management, positive social connections, and avoidance of risky substances.
It isn’t just the Space Force; in my role as a founding member of the U.S. Air Force Lifestyle & Performance Medicine Working Group since 2019, I have observed the Navy, Army, Coast Guard, National Guard, Reserves and Air Force integrating lifestyle medicine into clinical care at varying levels. Specifically, the Air Force has highlighted patient success stories using the six pillars, lifestyle medicine is being incorporated into military medicine residency programs and at least 75 clinicians across branches are now certified in lifestyle medicine.
Lifestyle behavior education and coaching are critical to U.S. service members, who may lack access to healthy foods, are disconnected from their families and friends, sleep on irregular schedules, encounter stressful situations and may be at increased risk of alcohol or other risky substance use. All service members undergo annual health assessments meant to identify significant health concerns which may impact military service and readiness, but often these are performed without a direct visit with the health professional team and may miss adequately addressing issues like poor nutrition, despite it being a leading cause of noncommunicable chronic disease.
The health assessments often include health recommendations but service members may not always read them or understand the critical nature of how food impacts health and military readiness. Additionally, lifestyle behavior changes usually require support from knowledgeable health clinicians to be successful, and the way the health assessments are accomplished may be missing opportunities to effectively engage service members on lifestyle issues.
To fully realize the benefits of a commitment to lifestyle medicine, we should invest to educate our military health care teams in therapeutic lifestyle behavior interventions and formalize consistent, evidence-based guidelines across all military branches. Time dedicated to topics like nutrition and physical activity is insufficient in medical education and continuing education curricula. As a result, many physicians and other health professionals are ill equipped to address these subjects with patients during clinical encounters.
Medical teams must speak a common language and understand the evidence supporting lifestyle behavior interventions to prescribe them effectively in a team-based, patient-centered manner. Studies show that clinicians who adopt lifestyle medicine health habits in their personal lives are more likely to discuss such behaviors with their patients, and their patients are more likely to adopt healthy behaviors. Education, supported by public information campaigns, can help build a culture of healthy lifestyle behavior by embedding the pillars of lifestyle medicine into training, operations and everyday life.
We shouldn’t wait. By prioritizing and investing in evidence-based lifestyle education now, we can begin to enhance our service members’ readiness, lower health care costs and ensure the brave individuals who protect us are physically and mentally prepared to complete the duties we ask of them.
Mary Anne Kiel, MD, FAAP, FACLM, DipABLM, is a board certified pediatrician and lifestyle medicine physician. She is former Air Force Patient Centered Medical Home Lead, former Chair of the Primary Care Clinical Community for The Defense Health Agency, and a current veteran champion of the Air Force Lifestyle & Performance Medicine Working Group.