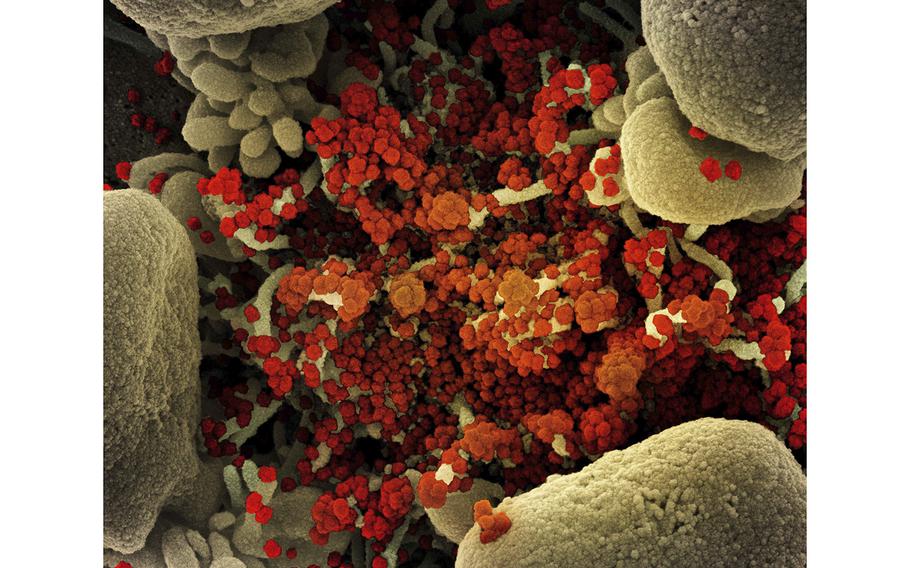
Colorized scanning electron micrograph of a cell heavily infected with SARS-CoV-2 virus particles (orange/red), isolated from a patient sample. The image was captured at the NIAID Integrated Research Facility (IRF). (NIAID)
Stars and Stripes is making stories on the coronavirus pandemic available free of charge. See more stories here. Sign up for our daily coronavirus newsletter here. Please support our journalism with a subscription.
With the U.S. headed into its third full winter of the pandemic amid fears that new variants will evade immunity from vaccines and prior infections, some scientists are seeking ways to blunt the coronavirus's slippery evolution by blocking the human proteins it uses against us.
If the strategy works, it has the potential to address several shortcomings of current treatments and vaccines, including their inability to prevent infections and maintain effectiveness in the face of a changing virus. The approach could also protect people with immune systems too weak to tolerate vaccines.
The virus depends on our proteins to make copies of itself and perform other functions. Shutting off its access to a crucial protein would be like depriving a predator of food or oxygen. Moreover, since some human proteins are hijacked by multiple viruses, a single treatment could be used to fight a broad spectrum of illnesses.
In the past month alone, two studies have appeared supporting the promise of targeting human proteins in treating COVID-19 — one published Tuesday in the journal Science Signaling, the other, which has yet to be peer-reviewed, posted on the science website bioRxiv.
But there is serious disagreement about the potential risk involved in disrupting our own proteins, and some scientists claim insufficient money has been committed to exploring this approach.
The $577 million in government funding devoted to speeding development of antivirals to combat COVID-19 excluded work targeting human proteins, said Charles Rice, a virologist at the Rockefeller University and winner of the 2020 Nobel Prize in medicine, along with two others, for the discovery of the hepatitis C virus.
"Many of us were quite disappointed with that exclusion," Rice said. "Both of those approaches should work and should be pursued."
Carl W. Dieffenbach, director of the Division of AIDS at the National Institute of Allergy and Infectious Diseases, defended the funding for the nine Antiviral Drug Discovery Centers, saying it addressed a "critical gap." He added that investigators can apply for grants to examine treatments that act on human proteins, an approach covered by a National Institutes of Health program called ACTIV.
"If you choose the right target, you can get things to work," Dieffenbach said, adding, "I have a healthy skepticism" about developing drugs that target human proteins.
He pointed out that both ivermectin and hydroxychloroquine target human proteins but have yet to show any value in fighting COVID-19. In addition, he said that aiming drugs at our own proteins "runs the significant risk of serious harm."
But others downplay the potential for harm, since treatment regimens for COVID-19 would be brief.
"Toxicity is much less of an issue if you take a drug just five days, instead of five years," said Nevan J. Krogan, an author of the study posted on bioRxiv and director of the Quantitative Biosciences Institute at the University of California at San Francisco. He stressed the importance of understanding and tailoring treatments to the specific actions of the virus.
Early in the pandemic, Krogan and a group of international collaborators mapped out hundreds of human proteins and the viral proteins that rely on them, and came up with a list of 69 compounds with the potential to disrupt those interactions. Almost 20 have entered clinical trials against COVID-19. Krogan is especially keen on one, plitidepsin, which comes from a species of sea squirt found only in the waters off the Spanish island of Ibiza. He said the drug has been effective in treating mice infected with each of the major coronavirus variants.
The Spanish pharmaceutical company PharmaMar has launched a Phase 3 clinical trial of plitidepsin, which is also being explored as a possible cancer treatment.
"The thing not widely understood is that for every disease except infectious diseases, we do target our own proteins," said Marc Feldmann, a professor emeritus at the University of Oxford. "Targeting the host is not unusual. It's absolutely routine."
One example is rheumatoid arthritis, the inflammatory disease that afflicts about 1.3 million Americans. The disease, in which the body's immune system attacks its own tissue, results in painful swelling and joint pain. Treatments target human proteins involved in inflammation.
To date, the U.S. Food and Drug Administration has given full approval to two COVID-19 treatments: the antiviral remdesivir, which is given intravenously to adults and some children, and the immune system regulator baricitinib, administered to some hospitalized adults. The agency has also granted emergency use authorization to several lab-made antibodies, as well as two antiviral pills, Paxlovid and Lagevrio, that can be taken at home by patients with mild to moderate COVID-19 to reduce the development of severe disease.
Doctors say there is a clear need for more treatments.
"My feeling is that we really need to focus on the host," said Otto Yang, associate chief of the division of infectious diseases at the David Geffen School of Medicine at UCLA. "Part of the reason we don't have better treatment is we don't fully understand the process leading to severe illness."
In particular, Yang said, more needs to be understood about the massive immune response called a cytokine storm, which often is what kills COVID-19 patients.
Raymond Dwek, emeritus director of the Oxford Glycobiology Institute, believes one key to potential treatments lies in preventing viral proteins from folding into the correct three-dimensional shape needed to bind to the receptors on our cells.
Since the virus does not have the protein-folding system it needs, it hijacks the machinery used by our own proteins.
This year, Dwek and others wrote in Proceedings of the National Academy of Sciences that seeking treatments aimed at our own proteins could enable scientists "to develop drugs with broad potential against viral families with pandemic potential, not only other coronaviruses."
Still, some scientists believe the virus will eventually defeat whatever barriers scientists erect.
"No matter what drug you approve, viruses will ultimately find a way around it," said Craig Wilen, an associate professor of laboratory medicine and immunobiology at Yale School of Medicine. For example, the drug might find another protein that can provide the same benefit as the blocked protein, just in a less efficient manner.
Wilen and other researchers believe that ultimately, the solution is likely to be a combination therapy, or cocktail, that cuts off the virus' escape options. Doctors already use this strategy to treat HIV and hepatitis C.
Developing a drug cocktail, however, raises other challenges, since it may require developers of different COVID-19 drugs to reach financial agreements.
"Trying to develop a combination therapy is more of a business challenge than a scientific challenge," Wilen said.